

Comparisons among groups used χ 2 testing for categorical variables and analysis of variance for continuous variables.
Continuous variables were presented as mean ± standard deviation. Categorical variables were presented as proportions and frequencies. Statistical analysisĬlinical and demographic characteristics among LDLT recipients and donors were stratified into three MELD score categories: MELD < 15, MELD 15–19, and MELD 20–24.

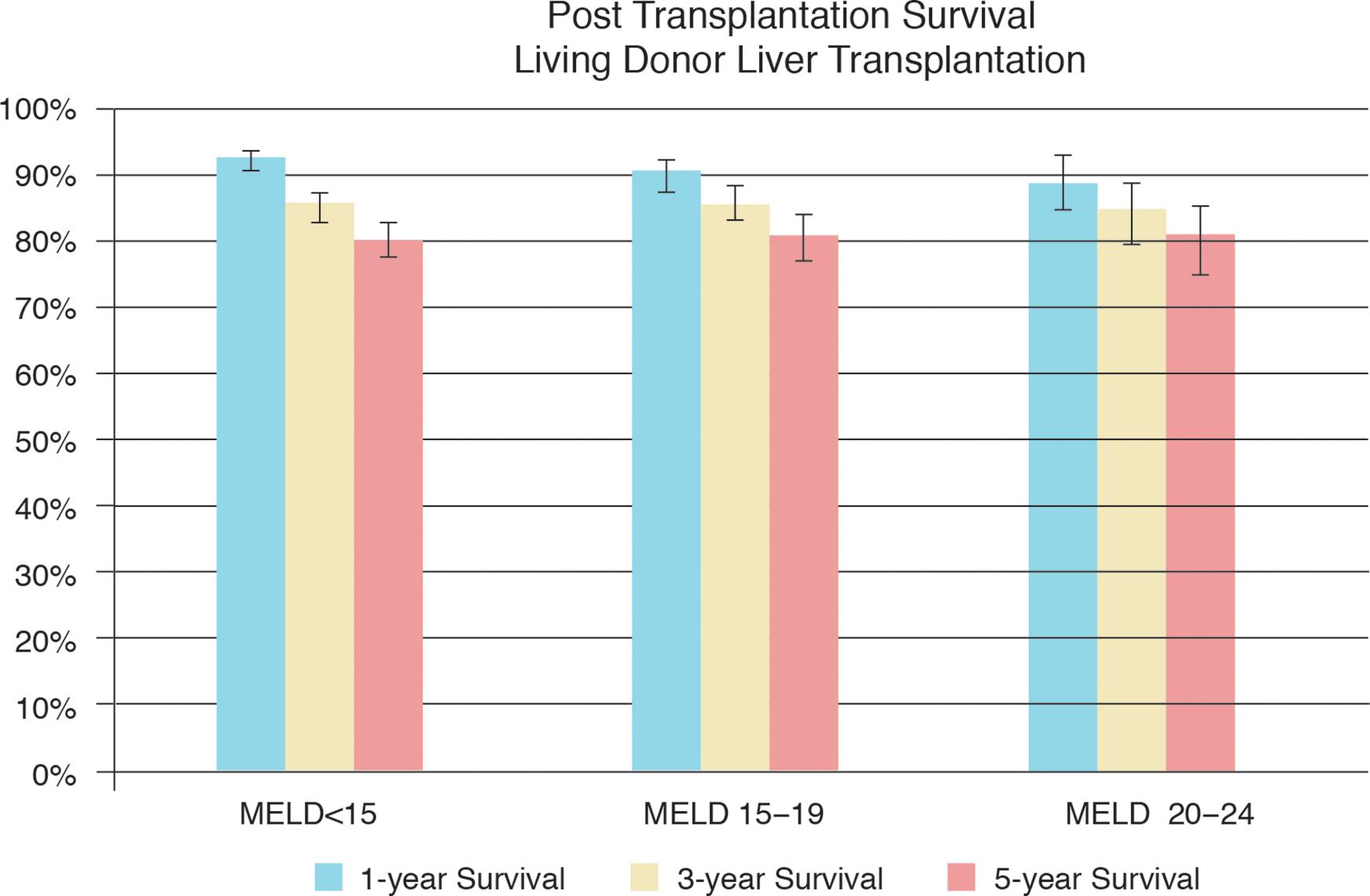
Data on graft-recipient weight ratio (GRWR) and graft weight/estimated standard liver weight (GW/ESLW) were not available. Additional clinical characteristics for recipients, including body mass index (BMI), obesity, hepatitis C virus (HCV) infection, hepatocellular carcinoma (HCC), ascites, hepatic encephalopathy, and diabetes mellitus (DM) were analyzed. Recipient and donor demographics were analyzed and included age at time of LDLT, sex, and race/ethnicity. from 1995 to 2012 were evaluated using data from the United Network for Organ Sharing/Organ Procurement Transplant Network (UNOS/OPTN) registry. Materials and Methods Study populationĪll adult patients (age 18 years and older) who underwent LDLT in the U.S. Therefore, the objective of our current study was to evaluate the association of MELD score and survival following LDLT in the U.S. This uncertainty stems from the paucity of large studies evaluating the effect of MELD score on survival following LDLT. Although the MELD score predicts liver transplantation waitlist survival, 5, 6 there is uncertainty surrounding what upper limit MELD score should be used to disqualify patients as too sick for LDLT. 2 – 4 However, it is unclear whether high MELD scores are even associated with lower survival following LDLT. MELD at transplant has been shown to be significantly lower among LDLT recipients compared to DDLT recipients. 1, 2 National trends reveal an aversion to offering LDLT to sicker patients with high Model for End-Stage Liver Disease (MELD) scores. 1 Despite comparable outcomes between living donor liver transplantation (LDLT) and DDLT, only 211, or 3.7%, of total U.S. In 2013, while 10,479 candidates were added to the liver transplant waiting list, only 5,921 liver transplants were performed in adults. Only 14% of LDLTs were performed in patients with MELD 20–24 and the remaining 86% in patients with MELD < 20.Ĭonclusion: LDLT is underutilized in patients with MELD 20 and higher.ĭeceased donor liver transplantation (DDLT) has not been able to keep pace with the increasing demand for liver transplantation in the United States (U.S.). When compared to patients with MELD < 15, there was no significant difference in long-term post-LDLT survival among those with MELD 15–19 (HR: 1.11, 95% CI: 0.85−1.45, p = 0.45) and a non-significant trend towards lower survival in patients with MELD 20–24 (HR: 1.28, 95% CI: 0.91−1.81, p = 0.16). Compared to patients with MELD < 15, overall 5-year survival following LDLT was similar among patients with MELD 15–19 (80.9% vs. Results: Overall, 2,258 patients underwent LDLT. MELD 20–24) and evaluated using Kaplan-Meier methods and multivariate Cox proportional hazards models. Survival following LDLT was stratified into three MELD categories (MELD < 15 vs. adult LDLT recipients with MELD < 25 were evaluated using the 1995–2012 United Network for Organ Sharing registry. We evaluated the association between recipient MELD score at the time of surgery and survival following LDLT. Background and Aims: Utilization of living donor liver transplantation (LDLT) and its relationship with recipient Model for End-Stage Liver Disease (MELD) needs further evaluation in the United States (U.S.).


 0 kommentar(er)
0 kommentar(er)
